TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
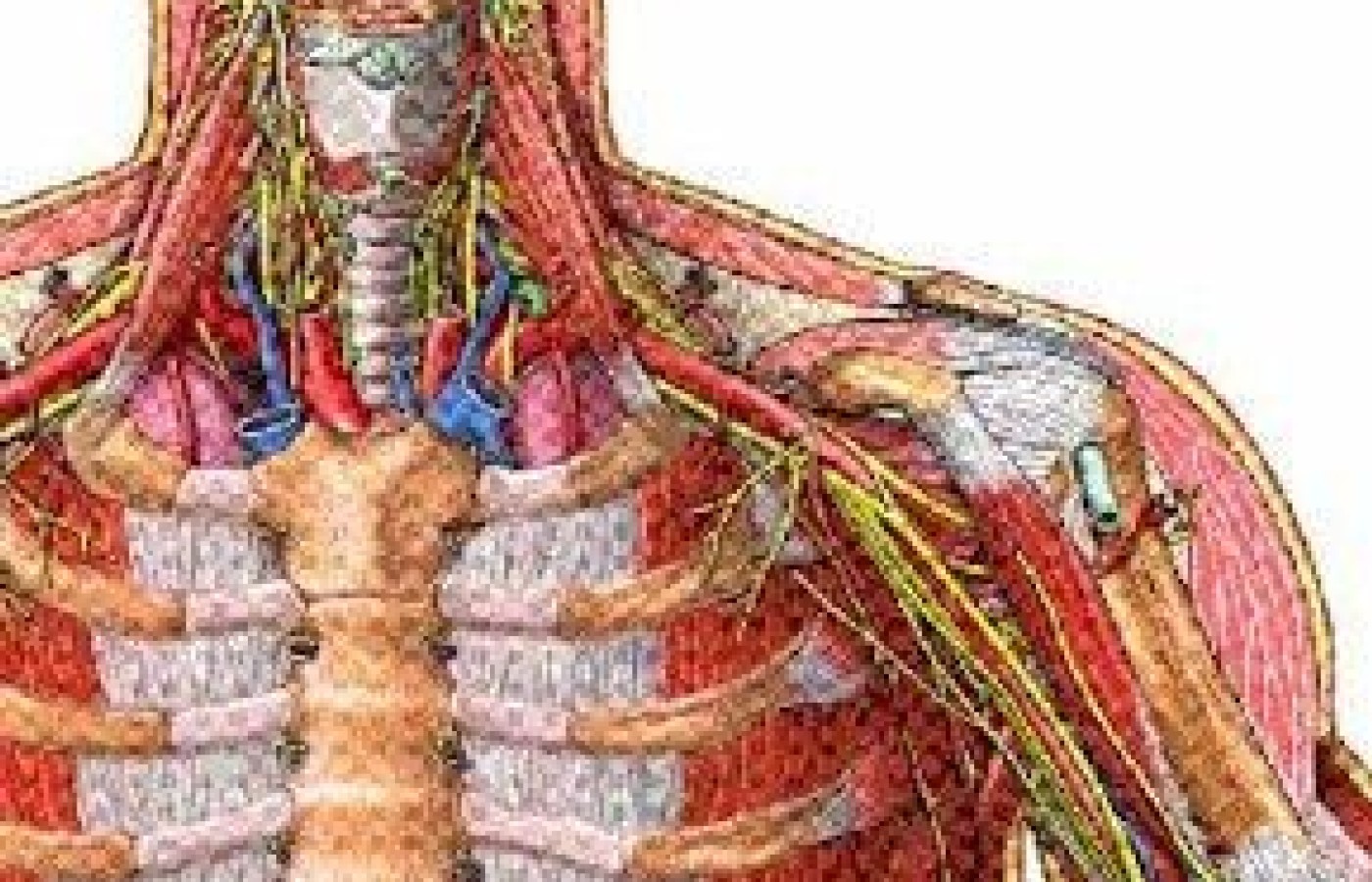
Thoracic Outlet Syndrome
Frequently orthopedists, neurologists or chiropractors refer patients with a diagnosis of thoracic outlet syndrome. This article will help you know what it is and how to treat it.
The symptoms of thoracic outlet syndrome (TOS) are pain, numbness and tingling of the upper extremity. The compression of the brachial plexus, subclavian artery and vein between the clavicle, first rib and the scalene muscles seems to be the cause. The nerves mostly affected are the radial; ulnar (90% of the cases); median; and musculoskeletal nerves. The patient's symptoms are pain/tingling/burning of the forearm/hand/fingers (third, fourth and fifth fingers). The pain medications usually prescribed include ibuprofen (600-800 mgs 2/3 times a day), naproxen (500 mgs two times/day), vioxx (12.5/25/50 mgs) or celebrex (100/200 mgs).
A diagnostic test that could be used for TOS is a nerve conduction study (NCS), which will show whether an abnormality is present (the test's results are usually inconsistent).
The examination is performed with the patient's head slightly extended and rotated toward the contralateral side of the area to be examined. Mild to moderate digital palpation is exerted on the scalene muscle rib insertion in order to find the active point(s) that will reproduce the patient's complaints (pain/numbness/burning or tingling, radiating to the upper extremity).

Technique used: Chinese acupuncture needles (#38 gauge).
Microcurrent device: Acutron Mentor, polarized pads, 50-75 microamps.
Pads: Zimmer disposable pads, single use.
Point combination: PC6 (if tender under light digital palpation) and/or SI3 connected with the trigger points (areas) of the anterior scalene insertion in the first rib (main points), and Liv4 and/or ST41 (secondary points). The secondary points are used contralateral (Master Tong technique), unless the ipsilateral points (same side) are more active: more tender to the palpation and reduces the pain more effectible than the contralateral ones. When palpating the scalene muscle insertion: look for the most tender (active) spots.
Treatment
The treatment frequency is 2-3 times a week for four weeks. The acupuncture needles are inserted with a slant direction (subcutaneous) with the microcurrent stimulation pads on top of the needles. The direction of the needles does not affect the treatment results.
The Acutron Mentor pads (polarized, with an output of 75 microamps, for 20 minutes) are applied directly on top of the needles. The positive pad is applied on the anterior scalene muscle insertion (needles and pads); the negative pad goes on PC6 or, more frequently, SI3 (needles and pads. Use the small size Zimmer pads combined with a .5 inch Chinese needle, #38 gauge, slant insertion). In the majority of the cases, the use of microcurrent is sub-sensational (the patient does not feel the electric stimulation). Some patients will feel a subtle local sensation (tingling, vibration, etc).
Improvement is usually felt within 8-10 treatments: pain, burning and tingling is diminished; pain medication is reduced or discontinued; and the upper extremity becomes more functional (daily activities are performed more easily than before). Stretching exercises targeting the scalene muscles are recommended to the patient to assist with recovery of the muscles and tendons. The stretching exercises should be done consistently, three times a day, no less than five repetitions per series. Stretching is maintained to the count of 5-10 seconds. Improving the patient's posture is essential for proper body biomechanics.