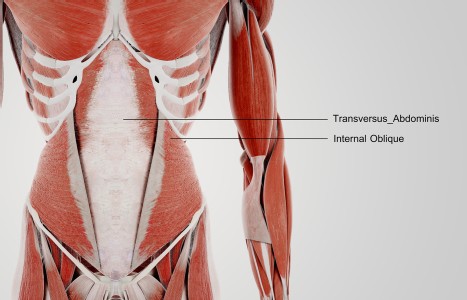
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Weighing the Costs
Acute combat-induced posttraumatic stress disorder (PTSD) is an anxiety disorder diagnosed in 24 percent of injured combat veterans serving in Iraq and Afghanistan.2 Onset of PTSD directly relates to multiple and lengthy combat-related deployments and trauma.5 Approximately one in six soldiers shows signs of PTSD on leaving Iraq and Afghanistan. Symptoms of PTSD include re-experiencing, avoidance behaviors, numbing responsivity and hyperarousal, as well as anxiety and insomnia. Unresolved PTSD becomes chronic and symptoms may continue for life.1
Advocates for the integrated approach in the treatment of PTSD at both Ft. Hood (El Paso, Texas) and Ft. Bliss (Killeen, Texas) were convinced that the traditional methods of treating PTSD weren't long enough in duration, intense enough or comprehensive enough. A program was created that would address all aspects of PTSD and treat the whole soldier. This integrative approach treats many of the symptoms of PTSD that are not addressed through the standard mental health protocols, including cognitive-behavioral therapy and pharmacotherapy. The concept eventually led to the implementation of the Ft. Bliss Restoration & Resilience Center and the Warrior Combat Stress Reset Program at Ft. Hood that incorporated medical massage, meditation, yoga, acupuncture, marital/family therapy and reiki with the standard treatment protocols of cognitive-behavioral and cathartic psychotherapies and pharmacotherapy.

The military relevance of these pilot programs can be viewed from an economic perspective. In a study conducted by RAND, researchers estimate that PTSD and depression among returning service members will cost the nation as much as $6.2 billion in the two years following deployment, including both direct medical care and costs for lost productivity and suicide.3 For a typical service person returning from Iraq or Afghanistan (an E-5 with 5 to 7 years of service), baseline scenario predicts that two-year post-deployment costs range from $5,635 to $13,935 for PTSD. If the service member did not improve from standard mental health care, they would be MEB'd. This means life-long veteran benefits that the Congressional Budget Office (CBO) estimates to be between $7 and $9 billion from 2008 through 2017 for Afghanistan and Iraq veterans. RAND estimates that the government could save as much as $1.7 billion, or $1,063 per returning veteran, through evidence-based research. The savings come from increases in productivity and reductions in the expected number of suicides. So far, the Pentagon has spent $5 million in 2008 researching alternative methods to treat troops suffering from combat stress or brain damage by using methods such as acupuncture, meditation, yoga and animal therapy.
Acupuncture can help reduce indirect costs and the cost of medical care, as evident in pain management. In a 2008 article, it was stated that the cost-savings for one week of outpatient acupuncture therapy for a single patient would be approximately $18.76.4 This includes the total cost for one week of pharmacotherapy utilizing celecoxib ($20.58), as compared to the cost of needles for one week of outpatient acupuncture treatment ($1.82). Additionally, the article also stated that there were 132 different patients seen at the outpatient acupuncture clinic. Thus, the total cost savings per patient for one week of treatments would be $2,476.32. Acupuncture treatments for pain management as compared to pharmacotherapy for one year would give us a total cost savings of $128,768.64. In terms of a reduction of indirect costs from outpatient acupuncture therapy, the article states that there was a decrease in sick quarters and light limited-duty status, resulting in an increase in operational man-days during Operation Iraqi Freedom.
References
- Kovach G. "Combat's inner cost." Newsweek. 2007;150(19).
- Hoge C, McGurk D, Thomas J, et al. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358(5):453.
- Tanielian T, Jaycox L (2008). Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Recovery. Arlington, Va.: RAND Corporation.
- Spira A. Acupuncture: A useful tool for health care in an operational medicine environment. Mil Med. 2008;173(7):629.
- Seale K, Bertenthal D, Miner C, et al. Bringing the war back home: Mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at department of veteran affairs facilities. Arch Intern Med. 2007;167:476.