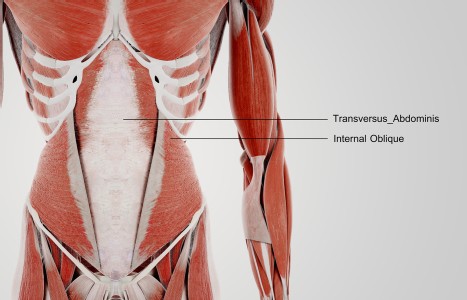
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
The Tests You Don't Have to Do
Let's face it, exams are a pain but necessary in patient care. Following a good consultation, a thorough exam will help you confirm your suspicions and document the patient's condition. We don't need to go into the whole realm of examination standards and protocols, let alone the scope of different diagnostic tests available. In the interest of time, we all want to get the most amount of information with the least amount of effort. I want to discuss two simple orthopedic tests you don't have to do. With the following tests, all you have to do is watch the patient.
First Test
When a patient has no lower back irritation, they will often sit right up after treatment - with no limiting pain or obvious discomfort. Amoss' Sign can be noted when the patient has pain rising from a reclined position. If they are lying supine they may turn to the side and use their arms to push themselves upright. The sign is considered positive if the patient indicates thoracic or thoracolumbar pain with the action of sitting up. This finding may indicate a spinal strain/sprain, intervertebral disc syndrome, or ankylosing spondylitis. Obviously, this is not a stand-alone diagnostic test - other testing should be done before you get to this point. If there are complaints of pain and other positive tests, this is also one more diagnostic finding you can add to your list of observed findings.
Second Test
If the patient is in a seated position, or has gotten up from lying down, also watch how they rise to a standing position. If the patient has complained of lower back pain or sciatica, they may rise by balancing on the unaffected leg and favoring the side of complaint. Such an observation is considered a positive Minor's Sign. They may also use one hand to hold the lower back and the other to push up from the table, also helping to reduce stress on the lower back. Again, this is an observed finding, not a physical test you perform - so watch your patient. This finding should be present with any lower back injury that causes muscular splinting in the lower back - sacroiliac lesions, lumbosacral strains and sprains, disc syndromes, etc. The degree of restriction will vary depending on the degree of the severity of the pathologic process.
Work With the Findings
Another way to use these tests is to evaluate for malingering. Some patients may present with acute pain - guarding all motion and screaming in pain at all the orthopedic testing you do, but then sit up and rise with no apparent pain. Such an observation should be a red flag for a patient that is not being entirely truthful about how they feel. Such a finding warrants further testing, evaluation, and possible referral for accurate assessment.
Since all you have to do is watch how the patient moves, it should be easy to add these tests into your exam protocol. Certainly there are other tests, signs, and observations to be made in the individual case.
The more information you have to confirm your findings, the more secure you will be in your diagnosis and treatment protocol. These extra notes help document the severity of the patients' complaints, and in a follow-up should show the progressive response to care. This extra documentation can also help make the difference if you must justify your diagnosis to an insurer or third party.
Take the extra few seconds to add these tests into your exam routine - they will serve you well.
References:
- Evans, R.C. (1994) Illustrated Essentials in Orthopedic Physical Assessment St. Louis, Missouri: Mosby.
- Hoppenfeld, S. (1976) Physical Examination of the Spine and Extremities San Mateo, CA: Appleton & Lange.