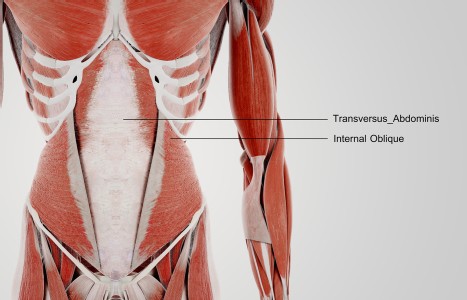
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
The Complex Journey of Healthcare Reform
Recent healthcare reform often referred to as "Obamacare" or the Patient Protection and Affordable Care Act (PPACA) was signed into law one year ago on March, 23 2010. The question today is does it have a future, or is it going to be repealed? What has the Department of Health and Human Services (DHHS) been doing to implement this law for the past year? How does the American public view the PPACA? How are we, as acupuncturists, affected by the legislation?
Two days after PPACA became law, Rep. Steve King (R-Iowa) introduced a bill, H.R. 4972, to repeal the Patient Protection and Affordable care Act, which was then sent to a number of committees for comment. Headlines lately have suggested that the law will be repealed, but in reality, this effort is very unlikely to ever make it through the Senate and pretty much amounts to political posturing. The opposition is attacking from a number of angles. A less lethal, but crippling blow would be to defund areas that involve healthcare reform, thus making the PPACA law ineffective. Fred Upton, the new chairman of the Energy and Commerce Committee, stated that the House will try to dismantle the law "piece by piece" and "we'll see if this thing will crumble."
Lawyers are challenging the constitutionality of the law in federal courthouses as Republican governors do the same thing at the state level - all the while taking millions in federal funds associated with healthcare reform for their state. Even states suing to nullify the law requiring most Americans to carry health insurance are proceeding with at least some of the building blocks. The challenge to PPACA constitutionality will be decided by the Supreme Court. However, the Court could simply choose to nullify parts of the law -- e.g., the disputed "individual mandate" to buy health insurance -- without necessarily overturning the entire law.

How does the average American feel about healthcare reform? Polls show that one in eight people believe they have been personally helped already, well before the meat of the legislation will kick in by 2014. 1 A recent Kaiser Family Foundation poll noted that one in five Americans said they were negatively affected by the law, citing cost specifically. Attitudes about PPACA have remained steady in the past year. Roughly half the American public polled - 53 percent- remain confused about the law while 47 percent responded that they lack sufficient information to clearly understand how it impacts them.
A Gallop poll released in March illustrated similar results according to whether "... the restructure of the American healthcare system is a good or bad thing;" 46 percent responded "good" while 44 percent responded "bad." Opinions remain sharply polarized along partisan lines where more than two thirds of Democrats support the law and most Republicans oppose it.2
One of the major issues with public opinion is that the majority of the legislation will not go into effect until 2014, leaving Americans to speculate and hear misleading sound bites cleverly produced by the opposition to create fear in the general public, for example that the law means a "government takeover of healthcare," a gross overstatement. A number of those polled believed the law has already been repealed. The truth is that no one can really predict the outcome of healthcare reform as it is currently written. If it's thoughtfully developed and well orchestrated, it can be one of the best things that could happen to our country this millennium. If it's poorly prepared for and mismanaged, it could be a complete debacle.
A Recap of The Past Year
There are 159 new agencies and programs born out of PPACA. Noteworthy steps forward include putting together the governing board of the Patient Centered Outcomes Research Institute (PCORI). Comparative Effectiveness Research (CER) is a huge step forward in the research community compared to the "gold standard" of Randomized Controlled Trials (RCTs), which are structured for pharmacological intervention. The HHS website defines CER as "the conduct and synthesis of systematic research comparing different interventions and strategies to prevent, diagnose, treat and monitor health conditions. The purpose of this research is to inform patients, providers, and decision-makers, responding to their expressed needs about which interventions are most effective for which patients under specific circumstances. To provide this information, comparative effectiveness research must assess a comprehensive array of health-related outcomes for diverse patient populations. Defined interventions compared may include medications, procedures, medical and assistive devices and technologies, behavioral change strategies, and delivery system interventions. This research necessitates the development, expansion, and use of a variety of data sources and methods to assess comparative effectiveness." The other pertinent advisory committee relating to AOM would be the National Healthcare Workforce Commission. That committee will evaluate the future needs of the nation and what multidisciplinary team of health care professionals is required to meet those needs.
According to the Office of Inspector General (OIG) report in February detailing top management and performance challenges of the Department of Health and Human Services for 2011, healthcare reform was one of the top four. The main issues pertaining to PPACA include: "...tight implementation timeframes; compliance with program rules; accuracy of claims data and payments; effective oversight of grants, contracts, and other obligations; quality of care; changes to Part D and other Medicare and Medicaid programs; and fraud schemes that put HHS and its beneficiaries at risk."
One of the highlights implemented this year is a 50 percent price cut on brand name prescription drugs for Medicare patients who fall into the coverage gap called the "donut hole." Republicans say much of these gains will be temporary. Sen. Orrin Hatch, (R-Utah) stated: "For families, any marginal benefits from this law are far outweighed by the heavy-handed intervention in their health care by Washington bureaucrats."
The proper implementation of the law will open the door to more reform, including the broad-spectrum use of complementary and alternative medicine. The current paradigm in the United States is one of "sick care" rather than 'health care," and we need to find a way to introduce more of a wellness focus to the system. The term wellness is frequently used, but rarely applied. Prevention and early detection are two very different approaches to improved health of our nation, and many lawmakers have referred to mammograms and colonoscopies as "prevention" which is misleading. Speaking of terminology, the moniker "integrated health practitioner" has been batted around for years with few legislators able to define it. Due to a task force assembled by the Integrated Healthcare Policy Consortium (IHPC), the definition was refined and issued in a press release on January 13, 2011 entitled "Policy Statement on the National Healthcare Workforce in an Era of Integration." The statement was as follows:
Seeking a balance between strongly held values of patient access to health care therapies and professionals of their choice and proper recourse if inappropriate or unethical care should occur, IHPC supports inclusion in the National Healthcare Workforce of:
1) All licensed conventional, complementary and alternative healthcare providers.
2) All state certified healthcare providers.
3) All nationally certified healthcare providers when the certification agency is accredited by the National Commission for Certifying Agencies (NCCA) of the Institute for Credentialing Excellence (ICE).
For healthcare professions that do not yet have state licensure/certification/registration or national certification, IHPC strongly encourages them to pursue state licensure/ certification/registration and/or national certification.
There are several areas in PPACA that refer to integrative healthcare. Given the new law, consumer popularity, the trend of major academic centers to be inclusive of integrative clinical centers and education in the medical school curriculum, and the potential of cost effectiveness, it is my contention that integrative healthcare will be an important and sustaining future trend in the redesign of healthcare delivery in the United States," said the chair of IHPC, Leonard Wisneski, MD, Author of "The Scientific Basis of Integrative Medicine."
So how does this statement affect AOM professionals? We obviously fall under the broad category of licensed healthcare providers (in 44 states and growing). The number of times "acupuncture," "chinese medicine," or "Oriental medicine" is cited in the entirety of the health reform law is zero. However, it provides a foot in the door - a place at the table for further conversation. AOM is integrated in a number of European countries' healthcare systems - it's about time America catches up.
However, the future for our profession is very bright.
A recent national health interview survey by the National Center for Complimentary and Alternative Medicine (NCCAM) at NIH show that the number of visits to acupuncturists rose by 32 percent in five years and that U.S. adults spent $33.9 billion out of pocket, a third of which were CAM practitioner costs. Additionally, there is rising concern about the number of physicians graduating, especially general practitioners/family practice MDs, in the future. In the past century, general practitioners grew with the local population. Now with more specialization, fewer MDs are choosing family medicine and projections suggest there will be a shortage of GPs from 2010 forward3.
AOM practitioners can assist in filling the gap. There are 65 accredited OM schools in America with over 8,000 students in the pipeline to serve the future public. Keep in mind that you will never be required to participate in insurance plans; just like today, it's purely your choice to remain a cash-based practitioner, or become a preferred provider.
References:
- Alonso-Zaldivar, R., "At first birthday, health overhaul faces uncertain future," The Salt Lake Tribune, Mar 21, 2011
- Blumenthal, M., "Health Reform Law: Same Opinions One Year Later," Huffington Post, Mar 25, 2011
- Colwill, J.M., Cultice, J.M., "The Future Supply of Family Physicians: Implications for Rural America," Health Affairs, 22, 1 (2003): 190-198