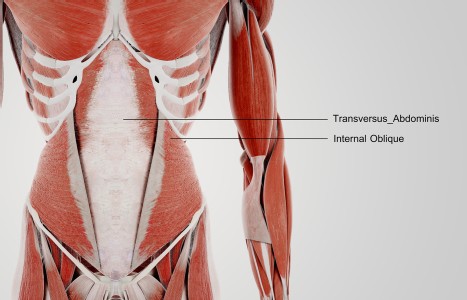
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Orchestrating Health With East-West Medicine: UCLA's Center for East-West Medicine Celebrates 25 Years
UCLA's Center for East-West Medicine (CEWM) was founded in 1993 as the vision of Dr. Ka-Kit Hui, MD. Based on a teamwork approach, the acupuncture training of Western practitioners was done by Dr. Hui in concert with physicians trained in Chinese medicine from China.
The Center today successfully combines outstanding clinical care, education, research, and international programs designed to advance the field of medicine and train the next generation of integrative medicine leaders. It has expanded to five outpatient clinic sites and an inpatient program at UCLA Santa Monica Medical Center. It is one of the most successful academic integrative medicine programs in the country.
In 2018, the clinics had 31,000 patient visits, with a majority of patient referrals coming from over 500 UCLA physicians. The clinics are staffed with 10 medical doctors, 3 East-West medicine clinical fellows, 10 licensed acupuncturists and a certified massage therapist.
Tsuda: What influenced your vision for the UCLA Center for East-West Medicine?

Hui: My dream was formulated back in the early 1970s when President Nixon went to China and was exposed to acupuncture used during surgery. At that time as a young medical student, I became aware that China had already embarked on this massive project of integrating Chinese and Western medicine to create a new medicine since 1955. I wanted to find a way to create this new medicine in the U.S. It started as an idea to develop a theoretical foundation for integrating Chinese and Western medicine to help improve clinical problem-solving, train more clinical team members and benefit people around the world.
Originally, most of our clinic patients were those who were not improving with standard medical treatment. I made the decision to originally focus on pain control when we started our clinical program. It was better to focus on clinical problems that Western medicine was not able to treat well. Because I've been a clinical pharmacologist, I personally do not like to use narcotics, and I think NSAIDS and steroids have a lot of side effects. I specifically chose to focus on myofascial pain and fibromyalgia because of the overlap between acupuncture points, trigger points and tender points. I believed this would be a good entry point for Chinese medicine.
Tsuda: What roles do licensed acupuncturists play in your center?
Hui: Acupuncturists have a very important role not only in the treatment of patients, but also to help build a team-based clinical program and to teach medical students, residents and fellows. I want medical doctors to know the value of acupuncture and work with acupuncturists as important team members.
Tsuda: Do you have any recommendations for licensed acupuncturists who want to get involved in integrative medicine?
Hui: First of all, I think they should really look into the Veterans Administration (VA). The VA is now able to hire licensed acupuncturists. In terms of how do people get into a system like UCLA, we want people who recognize how best to work within an institution that is very conservatively run by medical doctors. I've seen over the years that some acupuncturists work too independently and that creates a problem in terms of consistency and communication. Also, our clinics are very busy and very fast paced; so it's not like private practice where you work at your own pace. For an integrative medicine clinic to survive, let alone thrive, you have to be financially viable in addition to being legally defensible, socially acceptable and scientifically sound.
I think the acupuncture profession needs to have more awareness and training in the scientific basis for how acupuncture works mechanistically and be aware of clinical trial data. I want them to be well-versed in this domain. In addition to competency in acupuncture, to become part of a mainstream team you need to be able to communicate with non-TCM language, talk about the value of Chinese medicine and be able to participate in research discussions.
Tsuda: In terms of the next 25 years, what do you envision for CEWM and for integrative medicine in general?
Hui: With the high cost of care, it's my anticipation that Chinese medicine, acupuncture particularly, will become increasingly important. Just addressing chronic pain and the opiate crisis will increase demand and need for non-pharmacological, non-drug approaches. But, we need more people to understand that acupuncture is not just for pain control due to its concomitant effects on improving stress, sleep and other functions. I see a very bright future for Chinese medicine because stress and inflammation have been commonly seen in so many chronic diseases. That's where Chinese medicine comes into play; start out with something that's safe like acupuncture, tai chi, acupressure, and eating right. Chinese herbal medicine will also be very important but it would require more effort to build a team that knows about using herbs and drugs concomitantly.
In the next 25 years, I'm looking at what we can do to serve as the bridge; to bring together more team members to create what I call, the orchestra of health. There's no question in my mind that health care needs a new model and I think we have created a more person-centered, more preventative, more healing type of orientation and an educational self-care model that requires a variety of team members.
Whether you start from West or East, you need to look at what is the best medicine for the patient. It's more cost-effective when you teach people: how to do acupressure, do simple breathing exercises, learn meditation, how to eat right, and how to exercise and rest appropriately; you will add value to most clinical encounters. We need new primary care based team members, who know both East and West, to become the conductors of this orchestra.
I see that integrative medicine requires diversely trained teams to address the complex issues surrounding health care. Solutions for many conditions already exist; it's a matter of redesigning the health system and retooling health professionals. Realistically, it takes too long for people to be dually trained and have years of experience in applying this blended knowledge to clinical problem solving. So it's much more important for medical doctors to be aware of the potential of Chinese medicine, and feel comfortable working with other health professionals.