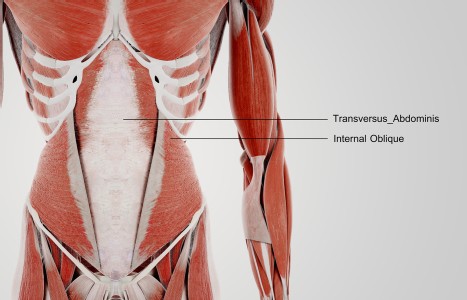
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Seasonal Allergies Relieved With Chinese Herbs and Acupuncture
Often referred to as "hay fever," allergic rhinitis can be caused by a variety of relatively harmless substances, ranging from pollen and dust to animal dander. The most common form of allergic rhinitis is seasonal allergic rhinitis, which typically occurs at the same time each year when certain plants are in bloom. Other people can be afflicted with perennial allergic rhinitis (which may occur at any given time of the year) or occupational allergic rhinitis (which is caused by an allergic reaction to substances in the workplace, such as chemicals or grains). All told, between 10 percent and 20 percent of the general population is believed to have some form of allergic rhinitis, with direct and indirect health care costs totaling between $4.5 and $7.7 billion per year in the U.S. alone.1
In China, acupuncture and herbal remedies have been used to combat symptoms similar to allergic rhinitis successfully for centuries. Previous research has shown, for instance, that Chinese herbal medicine can treat atopic dermatitis, while acupuncture has been proven effective in relieving the symptoms a number of allergic conditions. However, few studies have examined the combined use of acupuncture and Chinese herbal remedies in the treatment of allergic rhinitis.
A study in the September 2004 issue of Allergy has concluded that a combination of Chinese herbs and weekly acupuncture sessions may be more effective than a placebo at relieving the symptoms of seasonal allergic rhinitis. The authors of the study also suggest that future research be conducted to investigate the effectiveness of an acupuncture-herb combination in the treatment of other conditions.2
In the study, a total of 52 patients between the ages of 20 and 58, all diagnosed with seasonal allergic rhinitis, were randomly assigned to a traditional Chinese medicine group or a control group. In the TCM group, patients received a standardized 20-minute acupuncture treatment once a week for six weeks, with points on the Large Intestine, Gallbladder, Lung and Liver meridians stimulated. Additional points were selected based on each patient's individual symptoms. All of the patients were treated while in a supine position. After the needles were inserted, they were manipulated to obtain de qi. The needles were manipulated again 10 minutes after the start of treatment.
Along with acupuncture, TCM patients received a basic herbal formula (consisting of schizonepeta, chrysanthemum, cassia seed, plantago seed and tribulus), which they were instructed to take as a decoction three times per day, parallel to acupuncture treatment. In addition to the basic formula, every patient received a second formula tailored to the patient's individual TCM diagnosis.
In the control group, patients were given acupuncture at standardized non-acupuncture points distant from meridians, and were treated superficially with needles smaller than those used on the TCM patients. The needles were not manipulated, and the same points were needled at each acupuncture session. Control patients also received a non-specific herbal formula comprised of coix seed, licorice, poria, hops, oryza, barley, hawthorn fruit, and medicated leaven.
To measure the effect of each therapy, patients used a visual analogue scale to rate the severity of hay fever suffered during the previous week on a 10-point scale, and an assessment-of-change scale to measure any changes in symptoms. Patients also filled out an allergic rhinitis questionnaire to rate the severity of symptoms, and a pair of quality-of-life surveys. In addition, patients were asked to document the number of anti-allergy drugs taken for one week.
Patient Surveys Find Favorable Results for Acupuncture/Herb Combination
At the start of the study, visual analogue scores for each group were nearly identical (4.1 for the TCM group, 4.2 for the control group). By the end of the study period, however, the severity of hay fever was "significantly less pronounced in the TCM group" than in the control patients, and instances of remission (represented by a 0 or 1 on the visual analogue scale) occurred twice as often in TCM patients compared to patients in the control group.
Similar results were seen in the assessment-of-change scores and the rhinitis questionnaire. Improvement on the assessment-of-change score was observed in 85 percent of the TCM patients versus only 40 percent of control patients. An analysis of the rhinitis questionnaire, meanwhile, found that TCM patients experienced improvements in allergy symptoms in the eyes and nose, higher levels of physical activity, and an improved psychological condition compared to patients in the control group.
Intake of anti-allergy drugs also dropped dramatically among TCM patients. According to the researchers, "the permitted drug intake for allergic rhinitis symptoms decreased substantially, from 7.7 to 3.4 points in the TCM group, whereas we found only a slight decrease in the control group (7.7-6.0)."
The acupuncture-herb combination appeared to be well-tolerated by patients in both groups. Two patients in the TCM group complained of pain due to needle insertion, as did one patient in the control group. A second control patient complained of hematoma, while a third suffered from paresthesia in one arm, which persisted for 7 days. Five patients (two TCM, three control) complained that the herbal decoction either tasted bitter or made them feel nauseous. However, none of the patients experienced "severe or serious adverse events" that would have caused them to leave the trial.
Limitations and Conclusions
The scientists noted that their study methods contained some restrictions that might have impacted the quality of their research. For instance, they stated that one of the questionnaires used in the study may have been "methodologically inefficient" because of the potential for low patient compliance. In addition, the acupuncture-herb therapy used in the trial lasted only 6 weeks; other studies have indicated that longer treatment times and more individualized therapies have resulted in better patient outcomes.3,4
After taking the limitations into account, the authors suggested that the combination of acupuncture and an herbal decoction, tailored to the patient and administered according to the diagnostic principles of traditional Chinese medicine, could be effective in treating mild-to-moderate forms of seasonal allergic rhinitis. As they noted in the study's conclusion:
"We could show that this treatment was efficacious in improving global severity rating and in affecting disease-related quality of life parameters after 6 weeks of treatment when compared with sham needling plus a non-specific herbal formulation ... Taking into account the above-mentioned limitations of the study, we conclude that acupuncture plus Chinese herbal formulations may offer relief in patients with seasonal allergic rhinitis. Our findings support further investigations of acupuncture and Chinese herbal medicine in this and other diseases."
References
- Management of Allergic Rhinitis in the Working-Age Population . Summary, Evidence Report/Technology Assessment: Number 67. AHRQ Publication No. 03-E013, February 2003. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/clinic/epcsums/rhinworksum.htm.
- Brinkhaus R, Hummelsberger J, Kohnen R, et al. Acupuncture and Chinese herbal medicine in the treatment of patients with seasonal allergic rhinitis: a randomized-controlled clinical trial. Allergy 2004;59:953-960.
- Deadman P. The treatment of allergic rhinitis by acupuncture. J Chin Med 1991;36:25-27.
- Maciocia G. The Practice of Chinese Medicine. The Treatment of Diseases with Acupuncture and Chinese Herbs. London: Churchill Livingstone, 1994.