Did any of you ever get the feeling in school that it simply was not OK to speak about wanting to be successful? To get into the nitty gritty details of how to make money in practice? Maybe you were even someone like me who was directly told by someone in a position of power that I needed to take what I could get because in private practice, I wouldn’t make money.
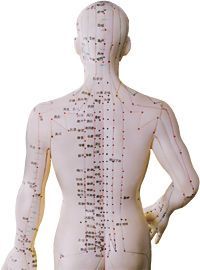
Acupuncture Found Effective for Back Pain
There seems to be no question that Americans spend a great deal of money dealing with back pain. According to research, we spend at least $37 billion annually on medical care for back pain.1,2 Furthermore, the economy suffers another $19.8 billion in lost worker productivity due to back pain.3
In response to this, there has been extensive research on the use of acupuncture for treating back pain. A 2008 literature review concluded that there was "strong evidence" for the use of acupuncture as an adjunct to conventional therapy for lower back pain.4 Now, a new study published in the May 11, 2009 issue of Archives of Internal Medicine has added even further to the literature on the value of acupuncture in treating back pain.5
Daniel C. Cherkin, PhD, and colleagues examined a group of 638 patients suffering from back pain to determine not only if acupuncture is superior to usual care for treating back pain, but to see if needle insertion at individualized points is the mechanism of action by which acupuncture works best. A total of 10 acupuncture treatments was provided over the course of eight weeks.
Study Design
The researchers started by dividing the patients into four groups:
Individualized acupuncture: This treatment was prescribed by the diagnostician at the beginning of each visit. There were no constraints on number of needles, depth of insertion or needle manipulation. Needles were retained for 18 minutes. Seventy-four distinct points were used.
Standardized acupuncture: This protocol used a standardized acupuncture prescription considered effective for chronic low back pain, including Du 3, Bladder 23 on either side, low back Ashi point, Bladder 40 on ether side and Kidney 3 on either side. All points were needled for 20 minutes, with needle stimulation at 10 minutes and again just prior to removal.
Simulated acupuncture: This technique used a toothpick in a needle guide tube. All acupuncture points were stimulated with toothpicks at 10 minutes and again at 20 minutes, just before they were "removed." The acupuncturists simulated insertion and removal of needles at the eight acupuncture points used in the standardized treatment.
Usual care: Participants in this group only received the care, if any, they and their physicians chose. This was mainly mostly medications, and primary care, and physical therapy visits. All participants received a self-care book with information on managing flare-ups, exercises and lifestyle modifications.
Results
At 8-week follow up, all groups of patients showed improvement. However, the "usual care" group only improved by 2.1 points (scored on a disability questionnaire), as opposed to the individualized, standardized and simulated acupuncture groups, which improved by 4.4, 4.5 and 4.4 points, respectively. The greater improvement for the acupuncture groups over usual care continued all the way to 52 weeks, at the end of the study. Of those patients receiving real acupuncture, only 11 reported any side effects.
Interestingly, at the end of the study, there was little difference between the four acupuncture treatment groups in terms of effectiveness. The researchers speculated that this may mean that acupuncture's actual mechanism of action may not be clear and that further research is warranted.
Nevertheless, they concluded, "Compared with usual care, individualized acupuncture, standardized acupuncture and simulated acupuncture had beneficial and persisting effects on chronic back pain. These treatments resulted in clinically meaningful improvements in function. ... For clinicians and patients seeking a relatively safe and effective treatment for a condition for which conventional treatments are often ineffective, various methods of acupuncture point stimulation appear to be reasonable options, even though the mechanism of action remains unclear.
According to Josephine P. Briggs, MD, director of the National Center for Complementary and Alternative Medicine, "The findings of this research show that acupuncture-like treatments, including simulated acupuncture, can elicit positive responses. This adds to the growing body of evidence that there is something meaningful taking place during acupuncture treatments outside of actual needling. Future research is needed to delve deeper into what is evoking these responses."
References
- Luo X, Pietrobon R, Sun SX, et al. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine. 2004 Jan 1;29(1):79-86.
- Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008 Feb 13;299(6):656-64.
- Stewart WF, Ricci JA, Chee E, et al. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003 Nov 12;290(18):2443-54.
- Yuan J, Purepong N, Kerr DP, et al. Effectiveness of acupuncture for low back pain: a systematic review. Spine. 2008 Nov 1;33(23):E887-900.
- Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009 May 11;169(9):858-66.


