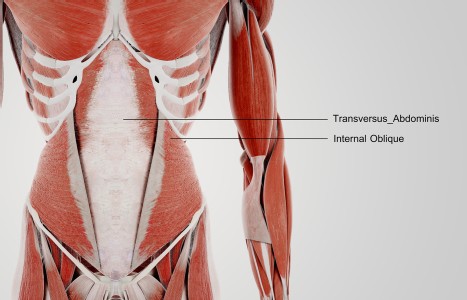
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Troubled Patients? Look For These Signs
I recently brainstormed the topic of troubled and/or psychotic clients with a group of close colleagues in different branches of bodywork and movement education. The exercise was invaluable. It highlighted the importance of a group discussion among health practitioners on the challenge of dealing with the unexpected, and in some cases, threatening actions of a client presenting irrational and/or potentially violent behavior.
We all agreed it was unwise to assume such clients only appeared in the offices of psychologists or psychiatrists. We also agreed that students in training in all our respective professions needed closer guidelines - heeding warning signs and red flags.
I would like to share three very different situations. I've altered names and locations to protect all individuals mentioned, as the incidents took place in the states and in different European cities. I've added my comments and advice in italics below.
Case 1 - Lenny
Even the most experienced among us can make mistakes. I was Skyped with "Joshua," who teaches a form of movement education globally. Joshua had just encountered a psychotic client "Lenny" referred by a local M.D. In an initial phone call, Lenny insisted on bringing his father, and asked if Joshua's wife Cecille could be there too, so the "group of them could talk."
Red Flag #1
Later, Joshua admitted in hindsight he should not have followed through with the appointment. The 28-year-old Lenny duly arrived with his father who joined Cecille in the clinic kitchen, while Joshua treated Lenny. After the session Lenny refused to leave, and insisted lying on the floor screaming. Finally he had to be handcuffed and removed by psychiatric paramedics and the police – after all knives or sharp objects were removed from the clinic kitchen. All of the above lasted some five hours.
"Five Hours?" I asked Joshua. "Impossible! How did your other patients react?" Fortunately no other patients were scheduled that day. Here's the story.
Lenny arrived and gave the appearance of being high on drugs, and claiming he was the "Buddha" and could "heal the world."
"I played along with him," said Joshua. "When I got him on the table he insisted on holding on to me and analyzing me, as I worked." Joshua soon realized Lenny was not high on drugs, but possibly bi-polar.
Red Flag #2.
The session should have ended right there. It would have been best to tell the patient this wasn't the appropriate moment for a session and enlist the help of Lenny's father to encourage him to leave.
When Lenny suddenly became psychotic, screaming on the floor and refusing to get up to leave, and his father couldn't handle the situation, the only available recourse was to call the emergency hotline.
Yes, the situation was disturbing for Joshua, an experienced professional and teacher of many years with a solid global reputation.
He reached out to close colleagues and Cecille to help him regain his own inner equilibrium. After a long hot shower and walk in the woods, he spent time cleansing the room with sage.
Hindsight: Joshua admitted he erred by assuming he was in control of a situation that could easily have escalated into violence. "As impossible and as difficult as it was," Joshua told me later, "it was very useful. It taught me about my own boundaries. It taught me to "walk-the-walk." I teach this all the time to my students. If something doesn't feel right during that initial phone call, don't book the appointment."
Case 2 - Joan
Picture a busy and popular group practice involving L.Ac's, Asian Bodywork Therapists and other professionals in complementary medicine. Team member "Lisa" acted instantly when she walked into the clinic one day and found a colleague's distraught patient "Joan" lying on the floor in front of the main desk shouting abusive things to a receptionist.
Lisa quickly determined that - a) Joan had pulled out her needles and rushed to the reception area while the attending L.Ac was treating another patient in another room - b) Joan's companion had gone to make phone calls and buy water.
Concerned about resolving a potentially volatile and public situation, Lisa asked someone to fetch the attending L.Ac, while she quietly knelt beside Joan. She reached for Joan's hand and held P6 and P8, all the time talking to her gently. This diffused the atmosphere instantly, calmed the patient, and eased the youthful receptionist's inability to handle the situation. Suddenly the attending L.Ac appeared out of one of the clinic room at the end of the corridor and came running toward them saying, "Don't touch Joan. She doesn't want to be touched." To which Joan responded, "I don't mind her touching me (meaning Lisa)– I don't want YOU to touch me."
At which point Joan's companion re-appeared with bottled water and said she intended taking Joan to the ER immediately. Lisa never found out the cause of the woman's volatile behavior – but suspected a possible reaction to medication, or some form of substance abuse.
To Lisa's surprise, the attending L.Ac reported her to the head of the clinic for "interfering" with his patient. In her own defense, Lisa said any responsible therapist would have acted as she did when confronted by a hostile and unpredictable situation in a public area in a busy clinic.
Hindsight: Lisa responded instantly to diffuse a volatile confrontation in a clinical setting, without giving a thought to her own personal safety. She was also concerned about the effect on other clients. It's a pity the L.Ac was more concerned about "losing face" than about acknowledging his mistake in needling a disturbed client and leaving her unattended.
Case 3 – Betsy
Shaun owns a popular dojo involving Asian Bodywork Therapy and the Martial Arts. He admits he found client "Betsy's" behavior a challenge during initial phone calls, and realizes he should have followed his gut reaction not to book an appointment
Red Flag #1
Betsy insisted on postponing the conversation, saying she was "cooking" or some other such excuse, and demanded to talk to Shaun at a time to suit her. She insisted on an immediate appointment, but was a no-show. No phone call. When Shaun finally reached her, Betsy said the lost appointment was not her fault.
Red Flag #2
Out of kindness, Shaun re-scheduled. Betsy appeared in his office sat across from him, removed her shirt and told him he had beautiful eyes. Shaun rose, told Betsy her behavior was inappropriate behavior and walked out of his office after politely asking her to put on her shirt and leave the clinic immediately. Betsy made a scene, and when asked to leave, began banging on the clinic door and shouting abusive comments. Shaun found her behavior threatening, but was reluctant to call the police. Finally Betsy left and Shaun breathed a sigh of relief. But it wasn't over. Betsy later tried to enlist her daughter in Shaun's martial arts classes for youngsters.
Red Flag#3
Hindsight: Shaun felt very sorry for the daughter and wasn't sure how to proceed although he felt reluctant to risk a situation that might prompt further confrontation with Betsy. My colleagues and I strongly advised Shaun to reject Betsy's application to enroll her daughter in his martial arts class. We advised him to discuss the situation with an official youth counselor if he felt Betsy's daughter was in any sort of danger.
Shaun agreed this was the best solution.
A final word. Let's continue to brainstorm such situations and share experiences with our colleagues in integrative medicine. I sense we would all find it helpful to encourage such group discussions to be included in our ongoing Continuing Education requirements. I welcome comments.