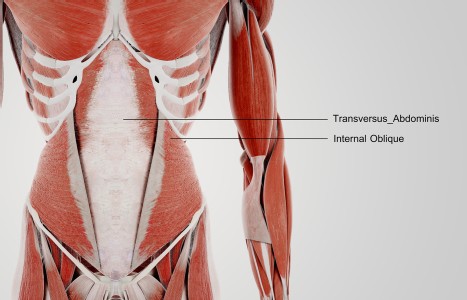
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
A Holistic Approach to Insomnia
Insomnia affects nearly one quarter of the global population. It is associated with mental health disorders, cardiovascular disease, and type 2 diabetes, among other health complications. Increased fatigue, impaired work productivity, reduced quality of life, and relationship dissatisfaction are also common in those with insomnia.
Approximately 6% to 20% of adults suffer from an insomnia disorder, which is characterized by persistent difficulty falling or staying asleep. This can increase the risk for health conditions such as heart disease and stroke, which can lead to death. Vgontzas, et al.,1 (2010) conducted interviews with 4,365 men and 12,219 women who were experiencing insomnia. They defined insomnia as less than six hours of sleep.
Associated Health Risks
People with insomnia are more likely to experience mental health issues including generalized anxiety, bipolar disorder, and major depressive disorder (MDD). It is important to note that insomnia is not secondary to the sleep disorder, but precedes the diagnosis. In addition, the response rate of people with MDD and insomnia is slower than those without insomnia.
“This study demonstrates the effect of insomnia on patients with MDD. According to ISI, HAMD, and SCL-90 scores, the sleep quality of MDD patients improved beginning in the second week and gradually improved with the increase of prognosis time. In addition, there is a recovery consistency between insomnia and MDD. It is a study to demonstrate that there is a clear correlation between insomnia and MDD.”
Postuma, et al.,2 (2019) studied idiopathic REM sleep behavior disorder (iRBD) as a predictor of Parkinson’s disease or dementia with Lewy bodies from 24 international sleep centers. RBD or iRBD is a sleep disorder or form of insomnia whereby a person has vivid dreams or nightmares that wake them up throughout the night. The researchers found that there is a correlation between iRBD and an increase in neurogenerative disorders. This tends to increase each year, as the prodromal period for neurodegenerative states can last up to 10 years.
Study: Acupuncture for Insomnia
An anecdotal study conducted in Tampa, Fla., collected data on 12 participants suffering with insomnia. Insomnia was varied in presentation, co-morbidities, and additional presentations. The participants differed in gender, age, race, and socioeconomic status.
Data was collected between January 2019 and October 2022. It included eight females (seven Caucasian and one African American); and four males, all Caucasian. The participants were ages 30-65. Health history information was collected through a thorough systems check from subjective, objective, assessment, and plan (SOAP) notes through electronic medical system.
Diagnosis was assigned to each participant delineating the type of insomnia specified to a traditional Chinese medicine (TCM) differential, as well as ICD codes. Participants may or may not have had other diagnoses, but they were not considered for this study. TCM acupuncture method techniques were applied; not five element or dry needling.
Results
Out of the 12 participants included in the study with a mean age of 46.91 years, 10 fully recovered after the treatment. The cadence of treatments was weekly and the number of treatments varied. Among the participants who fully recovered, some received as few as two treatments or as many as 14. Three patients received six treatments and one received 14. One patient discontinued treatment after receiving six with little results.
Delivery Systems: The Medical Model
What is the current medical model for minimizing insomnia? Cognitive behavioral therapy (CBT) is a psychological treatment designed to break patterns of maladaptive thinking and behavior, and has been known as a front-line treatment for insomnia. CBT comprises a behavioral component (stimulus control, sleep restriction, and relaxation) combined with a cognitive (managing sleep-related worries, racing mind, and intrusive thoughts) and an educational (sleep hygiene) component.
In a study by Norell-Clarke3 (2015), 64 participants with a diagnosis of insomnia and depressive disorder were randomized to receive either CBT or relaxation training (RT). There were primary outcome measures assessed pre-treatment and post-treatment at six months. Results showed that CBT is more effective at reducing insomnia, but equally effective as RT at reducing depressive symptoms.
Norell-Clarke states: “CBT was associated with less functional impairment, shorter sleep onset latency and wake after sleep onset but both treatments had equal improvements of sleep quality, early morning awakening, and total sleep time” (p. 90).
Bentley, et al.,4 (2022) studied two separate cost interventions for insomnia among caregivers for Alzheimer’s patients. One was CBT and the other mindfulness awareness practice (MAP). They looked at individual and group delivery, and discovered the most cost-effective was MAP. Cost differences were $3,978 and $1,981 for CBT vs. $1,884 and $1,377 for MAP.
One of the most current delivery systems for CBT is digital or DCBT. This is done using automated web platforms or a mobile app. Espie, et al.,5 (2019) studied the day and nighttime effects of insomnia. These included functional health status, psychological well-being, and patient-generated, sleep-related quality of life. They sought to improve areas of insomnia and personal functioning related to insomnia at 4, 8, and 24 weeks with 1,711 participants.
Treatment was structured into six sessions lasting 20 minutes each. They were personally tailored, and participants had access to the intervention for up to 12 weeks. Components included behavioral, cognitive, and educational interventions. Overall, this study showed not only that CBT is effective for insomnia and its daytime functioning effects, but also that digital CBT is effective. However, only 26% to 43% of patients achieve full remission from insomnia with CBT.
Embracing a Holistic Approach: Options
If traditional treatments are falling short, many are turning to complementary and alternative medicine (CAM) for relief. The National Health Interview Survey (NHIS) revealed that 1.6 million were using CAM to treat insomnia. These include acupuncture, herbs, and mind-body therapies such as meditation and yoga.
Ong, et al.,6 (2014) applied mindfulness meditation which is attention to the present moment as a vehicle to relax the nervous system. In post-treatment follow-up, the participants enjoyed an increase in 43.75 minutes of sleep.
Hartescu, et al.,7 (2015) executed increasing physical activity in a randomized, controlled trial involving 30 females. They recommended the amount of activity set forth by the public health guidelines. This consisted of less than 150 minutes of moderate to vigorous intensity physical activity per week, for six months. The baseline at 6 months reduction of insomnia symptoms decreased four points.
Williams, et al.,8 (2014) studied telephone intervention for obstructive sleep apnea (OSA). The study was a mixed methods approach. There was a two-arm randomized, controlled design to evaluate the effectiveness of a culturally and linguistically tailored telephone-delivered intervention with 340 Black participants at risk for sleep apnea who were randomly assigned to one of the two treatment conditions (170 in each). At the end of the trial researchers also conducted focus groups to assess participants’ overall impressions of the intervention.
Obstructive sleep apnea (OSA) is characterized by episodes of complete collapse of the airway or partial collapse with an associated decrease in oxygen saturation or arousal from sleep (Slowick et al., 2022).9 This results in fragmented, nonrestorative sleep which has implications for cardiovascular health, mental illness, quality of life, and driving safety.
The theoretical framework for the study was developed by Prochaska & Velicer10 (1997) and consisted of five stages the individual moves through to modify a problem behavior. The first stage begins with pre-contemplation, in which a person is not considering change and is often unaware that they have a problem to be modified; it continues to the maintenance stage, in which the individual has successfully altered the behavior (for six months or more) and concentrates on maintaining this new way of life.
Between these two stages, the person may contemplate change, prepare to change, and begin to act to initiate behavior change. This trial began in 2010 with 311 participants thus far. Although the intervention is designed to be practical and applicable, results are still inconclusive.
Zhou, et al.,11 (2022) studied three different interventions for sleep issues to determine differences in efficacy. In this single-blind, three-arm randomized clinical trial of 333 they sought to determine whether insomnia disorder can be treated effectively in the population over the internet and if intervention engagement can be increased. They utilized standard internet intervention (SHUTI) versus internet intervention that was culturally tailored (SHUTI-BWHS) and sleep education only.
They found that participants receiving SHUTI or SHUTI-BWHS had reductions in insomnia at a six-month follow-up. The greatest results were the ones who received SHUTI-BWHS, then those receiving SHUTI, and finally those receiving the patient education. The culturally tailored SHUTI-BWHS program was more effective at engaging participants with the program, as a greater proportion completed the full intervention. Program completion was associated with greater improvements in sleep.
Practical Takeaway
There are various holistic modalities to choose from for people suffering with insomnia. Acupuncture may be an effective modality in treating insomnia, regardless of the pattern. While the acupuncture study is promising, further studies are necessary to determine the specific mechanism of action with a larger and varied population.
References
- Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep, 2012;35(1):61-68.
- Postuma RB, Iranzo A, Hu M, et al. Risk and predictors of dementia and parkinsonism in idiopathic REM sleep behaviour disorder: a multicentre study. Brain, 2019;142(3):744-759.
- Norell-Clarke A, Jansson-Fröjmark M, Tillfors M, et al. Group cognitive behavioural therapy for insomnia: Effects on sleep and depressive symptomatology in a sample with comorbidity. Behav Res Ther, 2015;74:80-93. [url=https://doi.org/10.1016/j.brat.2015.09.005]https://doi.org/10.1016/j.brat.2015.09.005[/url]
- Bentley TGK, Castillo D, Sadeghi N, et al. Costs associated with treatment of insomnia in Alzheimer's disease caregivers: a comparison of mindfulness meditation and cognitive behavioral therapy for insomnia. BMC Health Services Res, 2022;22(1):231.
- Espie CA, Emsley R, Kyle SD, et al. Effect of digital cognitive behavioral therapy for insomnia on health, psychological well-being, and sleep-related quality of life: a randomized clinical trial. JAMA Psychiatry, 2019;76(1):21-30.
- Ong JC, Manber R, Segal Z, et al. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep, 2014;37(9):1553-1563.
- Hartescu I, Morgan K, Stevinson CD. Increased physical activity improves sleep and mood outcomes in inactive people with insomnia: a randomized controlled trial. J Sleep Res, 2015;24(5):526-534.
- Williams NJ, Jean-Louis G, Brown CD, et al. Telephone-delivered behavioral intervention among blacks with sleep apnea and metabolic syndrome: study protocol for a randomized controlled trial. Trials, 2014;15:225.
- Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea. StatPearls Publishing, 2022.
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promotion, 1997;12(1):38-48.
- Zhou ES, Ritterband LM, Bethea TN, et al. Effect of culturally tailored, internet-delivered cognitive behavioral therapy for insomnia in Black women: a randomized clinical trial. JAMA Psychiatry, 2022;79(6):538-549.