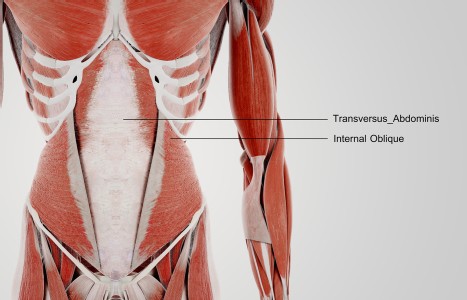
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Inside a DAOM Internship at a Level 1 Trauma Center
I recently had the pleasure of having a discussion with three individuals who practice acupuncture in a unique clinical and academic setting – providing acute care to hospital patients at Harborview Medical Center (HMC). For Bastyr University's Doctor of Acupuncture and Oriental Medicine (DAOM) students, a good portion of their clinical training takes place in Harborview's Pain Care Program.
Dr. Kathleen Lumiere, Bastyr DAOM program director; Dr. Erin Stewart, recent Bastyr DAOM graduate; and Brenda Loew, a much-respected instructor, practitioner, and also a current DAOM student, share their experiences working at the hospital's trauma center and developing this groundbreaking clinical training program.
Reddy: Please tell me about the genesis of your hospital internship program.
Lumiere: One of our clinical supervisors, Angie Hughes, met Dr. Ivan Lesnik, the director of Acute Pain Services at Harborview Medical Center (HMC) at University of Washington while working on an international clinic shift. Dr. Lesnik, who trained as a medical acupuncturist, subsequently reached out to Bastyr to fulfill part of his vision for an integrative pain service. When he described Acute Pain Services to me, it became apparent that - given the severity and complexity of the patient population, as well as the wide area to cover in the hospital - doctoral rather than master's students would be better able to meet the needs for high baseline clinical judgment and skills.

Doctors Lesnik, Gordon, Sturgeon, and myself, along with other faculty, staff and administrators within both institutions, helped to draft and approve the affiliation agreement between HMC and Bastyr. The cooperative nature of such a venture cannot be overstated. Training, privileging, onboarding, and operational details span multiple departments. The strong advocacy of doctors Lesnik and Gordon has been invaluable for creating and maintaining this collaboration, as well as the coordinated effort from Bastyr.
By the way, for your readers, HMC is a Level I trauma center, meaning that it staffs doctors, nurses and allied health professionals trained in emergency medicine/traumatology and surgery, and handles everything from severe injuries to car accidents and burn victims. HMC provides the highest level of surgical care available for trauma patients.
Reddy: Can you describe a typical "shift" at the hospital?
Stewart: The morning begins with a short discussion among our group members. We usually discuss any safety concerns, review special room precaution protocols and other acupuncture related topics. Then at 9 a.m. we meet for table rounds with the rest of the team that includes a spiritual care provider, psychologist, substance abuse/rehab provider, several internists, lead doctor, advanced registered nurse practitioner, physician's assistant, and pharmacy specialist.
We typically discuss each patient as a team to decide which patients would benefit most from acupuncture. Once we have the list of patients to see, the acupuncture supervisor assigns each student 3-5 patients to go visit, discuss the risks and benefits of acupuncture treatment, and potentially schedule a future appointment. The student also checks in with the patient's nurse to bring them into the loop. Each student ends up with 3-4 patients per shift, however there are some days when the patient load is lighter.
Reddy: Does the hospital currently employ acupuncturists? If so, what department(s)? Inpatient/Outpatient or both?
Stewart: Harborview does not employ acupuncturists at this time. This is primarily because Medicaid does not cover acupuncture and Medicaid patients comprise the majority of their patient base, and also because HMC is a University Hospital and the UW Medical School would need to approve such a move.
Reddy: What kind of outcome metrics are you measuring, if any?
Lumiere: Primarily a pain scale (0-10). An electronic medical record documentation template is used to document the procedure time-out, a brief history, tongue and pulse examination, TCM differential, pre-treatment pain assessment, details on treatment provided including points used and needle count, post-treatment assessment of pain, observations of note, complications and future plans.
Reddy: Did the program experience any "growing pains?"
Lumiere: Yes, although surprisingly few, which I credit to working with exceptionally reasonable, kind, and dedicated people. It took a while for a few of the doctoral students to reconcile some of their already considerable acupuncture skills with the clinical outcome research needs of HMC, and the environment of a hospital as opposed to a private clinic. A good working balance has been reached for the most part, and we are continually striving to make the program even better. This kind of reflection, course correction, and improvement just comes with the territory.
Reddy: What future do you see at this hospital system?
Lumiere: Ah. Well, already many other departments wish we could also provide acupuncture services for them, including Palliative Care. We are developing billing and compensation models so that Harborview, a publicly funded hospital, may be able to staff acupuncturists who would also be affiliated with Bastyr.
Reddy: Tell me a little bit about your focus on interprofessional education and leadership.
Lumiere: Our goal is to help licensed acupuncturists grow into highly skill-ed pain experts who can deliver excellent care under challenging circumstances, and communicate about what they are doing in a way that invites further gro-wth and collaboration between the professions. This has potentially far ranging benefits for patients and for practitioners, as well as for policy makers. Acupuncture is a cost-effective alternative, which we hope will not be "alternative" much longer.
Reddy: What professional growth have you seen with your students?
Lumiere: It's astounding! In two years I've seen them visibly grow into their roles as interdisciplinary pain experts, fluent in both acupuncture and biomedicine, some growing from having little confidence and experience to mentoring others and representing the best of our profession. I am very, very proud of them.
Reddy: Erin, how do you feel about the opportunity to train at a Level I trauma center?
Stewart: Practicing acupuncture in a fully integrated Western and Eastern hospital setting was a profound experience. Not only that, but the integration produces amazing results for the patients we see. On many occasions the nurses have expressed complete awe at the results we get with simple acupuncture needles. One nurse commented, "I wouldn't have believed it if I didn't see it with my own eyes" after I was able to reduce a patient's allodynia.
Reddy: Brenda, do you have any parting words for our readership?
Loew: Allopathic medicine has become more and more specialized and fragmented over time and there is now a genuine intent to combine the parts back into a "whole" by addressing the biopsychosocial and spiritual aspects of health and illness. Our being at HMC, regardless of limitations, is an attempt to do this and does feel as if it is a step in the right direction.
For readers seeking more info about Bastyr's DAOM program, or about developing hospital partnerships, please contact Angie Jordan, Program Supervisor, Bastyr University Dept. of Acupuncture and East Asian Medicine at ajordan@bastyr.edu, or at 425-602-3136.