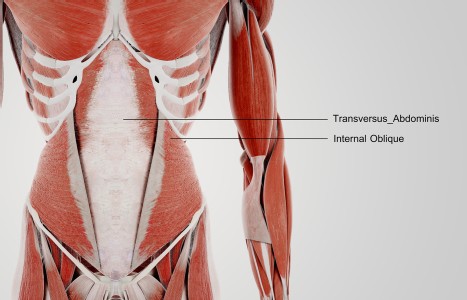
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Making Sense of Liver Regulation
In Chinese medicine, the liver has the function of moving and storing qi and blood. In its moving function, the liver smoothly distributes qi and blood to the tendons, muscles and flesh through microcirculation.
It also soothes and regulates the flow of qi and blood through the acupuncture channels and the blood vessels. In its function of storing blood, which happens in the early morning hours of 1- 3 a.m., the liver cleanses and detoxifies the blood.
Key Components
Liver regulation has key components that need to be evaluated and addressed: the movement of qi and blood; access to blood and yin; and the clearance of endogenous or exogenous heat.
Deficiency of blood or yin, or the presences of heat, will affect the primary function of moving qi and blood, basically contributing to liver stasis. Most patients with liver problems will present with some level of stasis of both liver qi and liver blood.
The main TCM term to describe the correction or adjustment of liver stagnation is "shu gan," which has been translated as "soothe, course, spread, or dredge" the liver. Here, the idea is to pull or push out liver stasis, which can be perceived like sludge.
Movement

Stagnation of liver qi and blood is a common clinical presentation when a patient first arrives at the clinic. It is best to move liver qi and blood, but at the same time, attention should be paid to whether there is enough liver blood, liver yin, and the presence of heat.
These variations should be addressed. Secondary considerations ask if liver stasis is overacting on stomach, spleen or uterus, or if there is the presence of liver yang or wind rising, or the unusual presentation of liver fire.
Etiology
Stagnation of liver occurs for a variety of reasons. Historically, TCM held that internalization of emotions, particularly anger and depression, could stagnate the movement of qi and blood. In this regard, internalization of emotional factors can lead to menstrual disorders such as dysmenorrhea and irregular menses; digestive disorders such as irritable bowel syndrome, gastric reflux and esophageal constriction; and channel syndromes including headache, anxiety, insomnia and inhibited sex drive.
Heat
Second, internal heat can lead to and aggravate liver stasis. This can develop from overconsumption of fatty foods, affecting both liver and gallbladder, or an overconsumption of refined carbohydrates, including sugars and alcohol.
The liver can also heat up due to environmental poisons in the air, food or water, and pharmaceutical drugs. These chemicals require liver enzymatic activity to metabolize, which releases heat. Heat can also develop due to a deficiency of liver yin or blood, both of which are necessary to cool the liver: yin by moistening and cooling the liver, and blood, which absorbs liver heat to help warm blood for distribution around the body.
Also, a woman's body increases in temperature between ovulation and menstruation, and this heat will aggravate any existing liver stasis. This is the etiology behind premenstrual syndrome.
Interrelationship of Stomach & Spleen
The third etiological factor behind liver stagnation involves its interrelationship with both stomach and spleen. One can imagine a vertical wheel consisting of spleen qi going upwards, with stomach qi going downwards.
A horizontal axis also exists between liver and stomach-spleen, and all three of these movements influence each other. If spleen qi is weak, or stomach loses its ability to descend downwards, these wheels can stop or slow down, and inhibit the smooth flowing of liver qi and blood.
Conversely, if liver is stagnant, it can affect the movement of spleen, stomach or both. Stagnation of liver qi, failure of stomach qi to descend, and deficiency of spleen qi can combine as one, two or three patterns. Symptoms of liver and stomach stagnation include bloating, epigastric or abdominal distension, esophageal reflux or constriction, nausea, vomiting and pain.
Blood Stagnation
Liver qi stagnation easily transforms into liver blood stagnation. When the qi and blood do not move smoothly, muscles and tendons become tight or tense. This is the mechanism responsible for irritability and headache, including symptoms found in premenstrual tension.
If the liver cannot smoothly deliver blood to the uterus, dysmenorrhea (menstrual cramping) and uterine fibroids can develop, as well as menstrual irregularity. Blood stagnation is the energetic etiology of cirrhosis (liver scarring), hepatomegaly (liver swelling) and splenomegaly (spleen swelling), which can follow the introduction of exogenous heat-toxins.
Liver stagnation that leads to liver yang flourishing upwards are treated with specific formulas to treat ascendant liver yang with internal wind.
Eight Formulas for Regulation
I would like to briefly discuss and differentiate eight commonly used formulas for regulating the liver. All of these formulas are available in product form from various manufacturers, and are included in my book Essential Chinese Formulas, which describes ingredients, applications and availability in detail.
One: Chai Hu Shu Gan San ("Bupleurum Dredge Liver Powder") is our basic foundation formula for stagnation of liver qi and blood. It was recorded by Zhang Jing-Yue in 1624, and is an enhancement of Zhong Zhong-Jing's Si Ni San (220 CE).
In this enhancement, three herbs move liver qi stasis: chai hu/Radix Bupleuri; xiang fu/Rhizoma Cyperi; and zhi ke/Fructus Citrus Aurantii, and two herbs move liver blood: chuan xiong/Rhizoma Ligusticum Chuanxiong; and bai shao/Radix Paeoniae Alba.
It is used for excess patterns, and is a very good foundation formula to clear excess when a patient first appears, arriving with mixed excess and deficiency patterns.
Two: Ge Xia Zhu Yu Tang ("Diaphragm, Below, Drive-Out Stasis Decoction") was created by Wang Qing-Ren in 1830. Wang created many formulas to address blood stasis. This formula is applied to blood stasis in the middle burner, particularly the liver (hepatomegaly) and the spleen (splenomegaly). It is effective in elevated enzymes due to hepatitis or cirrhosis, and can also be used for uterine blood stasis causing dysmenorrhea.
Three: Xiao Chai Hu Tang ("Minor Bupleurum Decoction") is a well-known formula from the Shang Han Lun (220 CE). The original application was for exogenous pathogen working it's way from the surface (taiyang) into the lymphatic level (shaoyang), and it is still used for this, as well as bringing herbs to the lymphatics.
Today it is also commonly used for a combined pattern of liver stasis with spleen qi deficiency, and in this regard it can be used to help regulate blood sugar problems.
Four:Xiao Yao San ("Free Wanderer Powder") was recorded by Chen Shi-Wen in the great imperial organization of Chinese herbal medicine in 1078. This formula addresses liver qi stagnation with underlying blood deficiency. It combines chai hu/Radix Bupleuri and bai shao/Radix Paeoniae Alba to move liver qi and blood, with dang gui/Radix Angelicae Sinensis to build blood. It can be used for chronic low-level liver stasis with blood deficiency, including post-menses, and elevated liver enzymes.
Five: Jia Wei Xiao Yao San ("Aded Ingredients Free Wanderer Powder") was built upon Xiao Yao San by Xue Li-Zhai in 1530. It adds two heat clearing herbs: mu dan pi/Radix-Cortex Moutan and zhi zi/Fructus Gardeniae. Heat can cause and aggravate liver stasis, and liver stasis in itself generates heat, further complicating the original stasis. This is the basic pattern causing premenstrual tension, and can also occur with accumulation of exogenous environmental poisons.
Six: Yi Guan Jian ("Single Linking Water-Decoction") addresses liver qi stasis with underlying yin deficiency. It was formulated by Wei Zhi-XIu in 1770. The liver moves qi and blood, but if heat develops, it can lead to stasis. Heat can generate just from normal liver activity. In modern terms, this includes heat generated by normal metabolism and detoxification on the enzymatic level. Liver yin, generated from kidney yin, helps keep the liver moist and cool.
If there is deficiency of yin, stasis can follow. Also, prolonged heat in the liver will deplete yin, again, aggravating stasis. Wu Bo-Ping, the great modern liver specialist, recommend this formula for regenerating liver tissue following damage such as Hepatitis C.
Seven: Shu Gan Wan ("Relax Liver Pill") is a modern patent medicine that moves liver qi while also descending stomach qi. It is a large formula (13 to 18 herbs, depending on the manufacturer) and is used for Liver overacting on Stomach. Symptom include abdominal bloating, nausea, costal distension, etc.
It is useful for excess patterns causing epigastric reflux, irritable bowel, and premenstrual abdominal distension. It is not recommend in digestive disorders due to deficiency of spleen qi.
Eight: Long Dan Xie Gan Tang ("Gentiana Drain Liver Decoction") was created by Wang Ang in 1682. It is the medicine of choice in excess liver fire, which can distribute throughout the liver and gall bladder channels (head, eyes, lips, costal, genital, inguinal), causing migraines, headaches, urinary disturbance, leukorrhea, etc. When combined with a good antiviral, anti heat-toxin formula, it is useful in acute episodes of both herpes simplex as well as varicella zoster (Shingles).
These major formulas should be thought of when confronting the more common liver presentations.