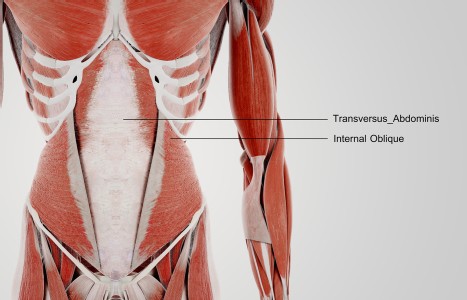
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Complex Cases: Tips for Navigating A Sacred Terrain
Have you ever had a case that felt so big you weren't sure how to wrap your brain around it? The challenge may have been diagnosis oriented: a progressed and debilitating autoimmune disorder, a degenerative neurological disease or metastatic cancer.
Other issues could have determined the difficulty such as low patient compliance, insufficient financial resources, a busy schedule, demanding workload or young children. Perhaps there was a physician who felt your contributions were a hindrance to the patient's care.
There are many reasons why a case can feel daunting.
We all have patients who push the envelope of our expertise and require that we expand the way we work. If you have ever felt overwhelmed by such a case, you are not alone. Patients like this pop up in everybody's practice. They don't discriminate against the new practitioner either. Those of us who have been practicing for decades run into them head-on also. No matter how much you revere your teachers, even they need to partner up with humility and new strategies when it comes to tough cases.
I am going to share some of the tools that I have come up with to help me navigate this difficult terrain. Perhaps some of these ideas will be helpful to you. I will take on a case if I feel I have a real shot at being successful with it. I don't put that responsibility only on my own shoulders, though. I like to split it with a patient. Here is how I divide that responsibility.
At the first session I do my diagnostic work and come up with what I call an "energetic profile," the condition of my patient's qi, the snapshot, the diagnosis. After I share my findings I send them home to seriously think about their budget for healing the condition.
Their Budget Determines Outcomes
I tell my patient that healing their condition is a project that will take time and money and is an investment in their future. Rather than pushing for higher levels of commitment than my patient can make as I spend months trying to get results, I find out what they can put into their healing up front.
My budgets are made up of three things: dollars, hours and miles. How many dollars does the patient have per day, week or month to invest in healing the problem they are presenting? How many hours do they have per day, week, month and how many miles will they travel to get well? The answers vary tremendously and give me the foundation I need to build an effective treatment protocol or to tell them that I am not the best person to work with them. When I have clarity about their level of participation I can better asses the likelihood of getting results with the resources they have available. I don't want to be badgering a patient to do more and I don't want to fail because I can't get results with the amount of commitment my patient can make.
Some patients have lots of dollars to devote to a problem but not very much time. These folks are highly committed making the money they then use to heal. On the other hand, some people with fewer financial resources may have more time to contribute. This is not always the case and one is not generically better than the other. It's just good to know what I have to work with and find the advantages in every circumstance.
A patient's budget doesn't have to be static and can change by the week or month. Parents may need to have different budgets when children aren't in school, for example, or if they lose a job. I may be able to work with the changes if I have an idea of what they will be and can prepare for them. But surprises in patient involvement don't work well with complex cases so I always ask my patients to give me notice of budget changes well in advance.
I include miles in the budget because I need to know if I can send someone to a physician, healing center or seminar out of town. One of my favorite homeopathic physicians is in Oregon. Is my patient willing to fly there if I feel that this particular ND would be helpful? The Hoffman Quadrinity process, (Hoffmaninstitue.org) is the most brilliant seminar I have ever sent patients to if they need to learn about how childhood experiences and trauma influence their health and body-oriented lifestyle decisions. These seminars are in 15 countries around the world, including the U.S. Will a patient fly to Napa Valley, Calif. to experience this life transforming opportunity? I have many examples of this nature. My favorite foot surgeon is in Arizona, my favorite integrative medicine hospital is in Philadelphia, etc. Miles could also refer to how far a patient will go locally. If they rely on public transpiration can they get themselves to the physical therapist who specializes in their condition but is 20 miles away or should we stay more local?
Upon examination of a budget I may see that a patient doesn't have the resources to see me as often as I consider necessary. I may decide to offer them a lower rate to allow for my greater involvement or I can become a monthly or quarterly advisor, a manager of sorts. I assume the role of the less frequent, but consistent team organizer whose network of resources helps maximize a patient's limited resources.
Set Realistic Expectations
When a patient gives me their budget I can give them better time estimates and appropriate expectations. One strategy, that has never failed me, is that of informing a patient that their body takes time to "show" results and that they need to commit to coming for a minimum of six treatments before they expect to see any improvement. "If you aren't comfortable doing that, let's not get started," I tell them. Much of what we do is below the surface. It may take many treatments before a seriously ill patient improves to such a degree that they notice benefit from your work. The first few weeks or months may not feel any different to them. By telling my patient that the healing rate is dependent upon his or her own body's ability to metabolize our work I take the inappropriate expectation of speeding up the process. I have never needed six sessions for patients to notice results but I still like to give the process this lengthy window. The longest I have needed was five sessions and that was with a severely qi and blood stagnant elderly gentleman. Stagnation takes a while. When patients get results in less than six sessions they get excited about our progress rather than frustrated with how long it took to start feeling better.
Give Little Jobs
When someone is severely ill they want to do something between sessions that will help them get better. This is empowering and uplifting to their spirits while gently supportive of your work. Because their energy is severely compromised they are likely to tire, feel pain or overwhelm relatively quickly, so it is best to make those jobs small. Have one appointment with a specialist, walk for five minutes a day or every other day. Supplement and herb dosages must be small too.
Handing someone ten bottles of herbs, nutrients and homeopathics early in the treatment process and suggesting multiple dosages a day may backfire. Remember, our medicine works under the premise that you give a patient dosages in proportion to what they can metabolize, not in alignment with what they need. The body's need level is high in severe illness but its absorption and utilization ability is generally low. Give the body less and be patient. This is the way of our professional ancestors. Low dosages that build over time help big problems go away at an appropriate pace. This yin method of healing is important when undertaking the major transformation required in cases of this nature.
Remember the Sanctity Herein
Working with heavy duty, complex cases can keep you up at night thinking these cases are rewarding and an opportunity to dive deeply into the beauty of OM. Its richness shows up in many subtle and unique ways. I am reminded of the genius in this medicine, the generations of effort that have gone into its creation and refinement, when I unravel a complex puzzle of energetic syndromes over the course of years. I recall the first time a patient smiled at me, seven months into the course of treatment. After 25 years, eight surgeries and continual worsening from rheumatoid arthritis, she felt better enough to smile. And the deep sighs expressed by a patient whose severe diaphragmatic spasm had kept her from breathing deeply for over a decade. It is the details that first express the light of our medicine.
I hope you come to enjoy the challenges that are inherent in treating patients with severe illness. As your work has impact, layers of energetic disharmony dissolve into the body's beautiful music and harmonious vitality. Life hungers for itself. Life yearns to flow into and regenerate itself. It's a miracle to behold and an honor to participate. May we all be blessed in such sacred undertakings.