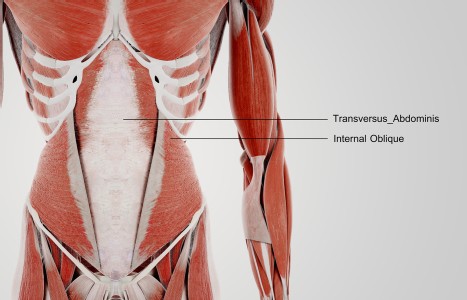
TrA-2, my primary needle location, I needle 95% of the time and I think it works the best. You’ll know you have the right point location when you discover the muscle twitching when applying electric stimulation.
Communicating With Your Patients About Pain
Presumably you speak the same language as your patients do. Still, communicating about pain can be difficult. There's more to it than finding out if the pain is sharp, dull, stabbing, throbbing, constant, coming and going, hot, cold, etc. There may be even more to it than asking whether or not the pain interferes with the patient's daily activities. There are some alternate pain scales and ideas that can be helpful when our patients are trying to communicate with us about pain.
However, pain scales don't always tell the truth. People are used to being asked about their pain on a scale from 1-10. But, does a pain level of 6 mean the same to your patient as it does to you?, not necessarily. Do numbers really help get the point across? I suppose if the person says "this one goes to 11" you might get the idea that the pain is really high. But, what if they explain their pain with drawings and words? The Mankoski pain scale provides words as well as numbers to get the point across. A 6 on that scale is "Can't be ignored for any length of time, but you can still go to work and participate in social activities. Stronger painkillers (codeine, narcotics) reduce pain for 3-4 hours."
Another pain scale used in a blog named "Hyperbole and a Half" uses illustrations that go beyond happy and sad faces. While it may not be something you want to hang up in your treatment room, the accompanying drawings are very graphic interpretations of pain. A 6 on that scale shows a person with tears starting to well up in their eyes. The description for number 6 says "Ow. Okay, my pain is super legit now."
The Spoon Theory
Are you familiar with the Spoon Theory by Christine Miserandino? Spoons are not just for eating. If a patient comes into your clinic and says "I'm all out of spoons" do you direct them to the nearest housewares store? If not, I highly encourage you to read about it. In it, a woman explains to a friend what it's like to live with Lupus using an analogy of starting out each day with a set number of "spoons." You can replace "spoons" with qi to apply it to Chinese Medicine.
People with chronic pain and illness often have to really work to conserve their qi/spoons in order to get through the day. For them, it may take more qi than it does for a healthy person to get through their daily tasks. The Spoon Theory is not just specific to people with Lupus. It resonates with many people who have chronic illness and pain conditions.
When a patient starts to talk about their pain level, listen now and write more later. When a patient comes in for the first time and tells you about the pain they're experiencing, you may be writing or typing your notes furiously. While it is important to write down information it's even more important to look and see where the patient is experiencing pain and listen to them when they talk about it. You may also want to restate what you heard the patient describe and ask if they agree or disagree. This will help clarify your understanding of where and how they experience the pain.
Details, details
The more detailed description a patient can give you the better. Being an acupuncturist is a bit like detective work. Sometimes all the clues are right there in front of you when a patient can accurately communicate to you about how they're feeling. Sometimes you have to dig deeper to find the clues and ask more questions so you understand.
Check in with your patients. You may get subtle clues about their pain from breathing, body language, and even how they walk in and out of your office. It's important to check in with your patient during and after their treatment to see how they respond and whether their pain has increased, decreased or remained the same.
If you haven't heard from a patient in a while after their appointment, call or email them to check in and see how they're doing. It's possible that they're not experiencing pain and they forgot to tell you. Or it's possible that the pain hasn't changed and they don't know how to tell you. You won't know if you don't ask.
Emphasize the importance of nutrition when assessing pain. Refined flours and sugars can often make pain worse. I usually ask my patients to cut back on their consumption of refined foods because asking anyone to cut them out all together is a very drastic change and may not be realistic. Usually when patients see how cutting back on certain foods helps their health, they're more likely to stick with the change and make it a lifestyle choice, rather than think of it as a burden.
Be Patient
You do not have a crystal ball, so set realistic expectations. While you may be able to make a difference in one acupuncture session, don't predict how long it will take until your patient sees results. While pain conditions often show improvement more quickly than other ailments, that isn't always the case; sometimes pain conditions are slow to show results.
You can be sympathetic without being empathetic. We want to make a difference in our patients' lives. Indeed, that's why some of us become acupuncturists. You don't have to have experience in all the different kinds of pains your patients present in order to treat them, but you can be compassionate about it. How you respond to a patient who comes to see you and is crying from the pain makes a lot of difference. If you can't help them, ask your colleagues for help or refer them to another practitioner.
Our patients want to be heard. If you give them the chance, they'll tell you a lot of information about their pain and how they feel about it. Use some of the alternative pain scales and ideas that people in pain have come up with when talking with your patients. This will not only help you understand what's going on but will also help you make a better differential diagnosis and become a better practitioner.